My Family: We stay together
My husband and our two sons, Drew and Ben, all have the same tattoo on their upper arm: a lion, a red shield, and the letters of our family name, Dooley. They got the tattoos in 2009, while they were working on our house. It took them then three years to completely finish it. They worked really hard at it. My husband took night shifts at the post office so that he could be on the construction site during the day. Drew came over after work. Ben was still in school and helped mostly during vacations. The close teamwork brought the three of them together. I don't have a tattoo, but I never forget that family is the most important thing in life. Family: that's not just my husband, not just my children. It's all of my other relatives too. Family of course included Tim's mother, LaVonne. There is this cliché of the wife not getting along with the mother-in-law, but that was never the case with me. I've always admired LaVonne: a bold, cheerful woman who enjoyed life. She learned to drive a car at age 68. And when I think of her, I usually remember her cooking: cooking made her happy. LaVonne, standing in her kitchen and preparing a turkey.
„You have to teach them a lot, but you can learn a lot from them, too. Joy about the little things, for example: how good an apple tastes, how funny the dog looks when he yawns.“
Cooking bacon on a gas stove while camping. LaVonne had a stroke, right on her 80th birthday. Part of her brain was irreparably damaged. Her right side was paralyzed. She could no longer walk, she could barely speak, she couldn't chew or swallow. Her husband Marv was already 83 at the time, but he took care of her at home for eleven long years. Because I was with LaVonne four days a week during the final months, I know how hard and difficult this work was. LaVonne couldn't control her bladder, so she had a catheter. She also frequently had problems with digestion. She had to be fed artificially, her clothes, diapers and linens had to be changed and her body had to be washed and moved. When LaVonne died in the spring of 2017, it was a release for her and for all of us. I think of her often. How her eyes sparkled once when I trimmed her fingernails and said: "The marvelous meals these hands have cooked." How she looked at her grandchildren from her wheelchair. How she made a half-amused, half-annoyed gesture with her hand when Marv joked with her and said, "Tomorrow we'll finally go camping again."
And, of course, how lovingly Marv attended to her, every single day, every second. We often suggested that he should put LaVonne in a nursing home. But for Marv, it was out of the question. He said: We stay together, in good times and bad.
Offering a Better Way
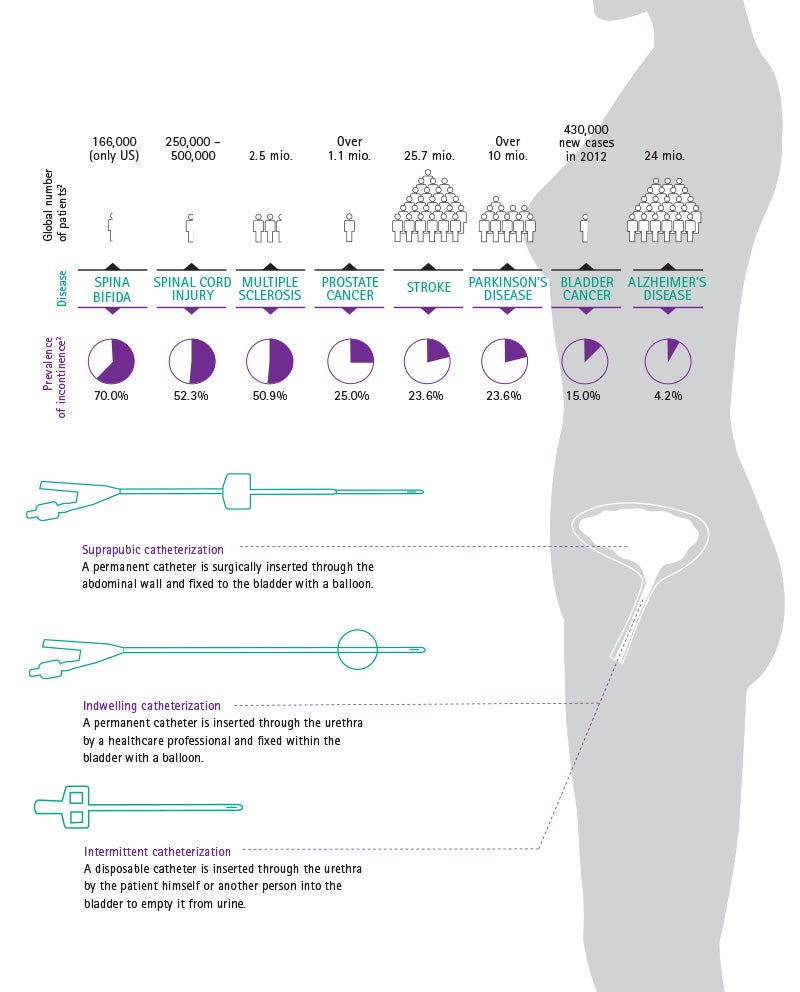
Continence care and urology | Urinary disorders, incontinence or retention affect millions of people all over the world. In the USA, 14 percent of all men suffer from urinary incontinence and 51 percent of all women, who are affected more than men due to their anatomy.1 Urinary disorders can have many different causes, can develop in varying degrees of severity, and occur in both acute and chronic forms. However, modern medicine offers remedies for even the most severe cases.
Three methods for bladder emptying
In many patients, the neurologic control of the sphincter and pelvic floor muscles is impaired or even non-existent. The reasons for this can be spinal cord injury, multiple sclerosis, spina bifida, prostate or bladder cancer, but also stroke or Alzheimer's disease. The consequences: the urine either remains in the bladder or is emptied uncontrollably – in either case, a urinary catheter is necessary.
The most common is the so-called intermittent catheterization technique with a disposable catheter. Used four to six times a day, a thin tube with drainage holes, called catheter, is inserted through the urethra to the bladder to empty it from urine. It could be performed by healthcare professionals or the patient himself. The second technique is with the indwelling foley catheter. This type of catheter is inserted through the urethra and fixed within the bladder with the balloon positioned on the top of the catheter. It should be connected to a urine bag for continuous urine collection. This catheter can remain in place for days or weeks. However, permanent catheters are associated with a higher risk of urinary tract infection and should be used only when no other bladder management method is available. In the third catheterization method, the suprapubic method, the catheter is inserted through the abdominal wall instead of the urethra. This method is performed when the urethra is pathologically narrowed, blocked, or after surgical interventions, in particular within a posttraumatic context.
B. Braun solutions for all three methods
When suprapubic catheters are used, it is particularly important to insert them as carefully as possible through the abdominal wall. The Cystofix® SG system enables this, with cannulae that have a diameter of only 1.3 millimeters. The Urimed® Cath combined with the Uro-Tainer®, the urological flushing solution, has proven successful for use as a permanent catheter management reducing blockage and incrustations. For the intermittent method, we offer our Actreen® catheter product line. We also offer the set version (preconnected catheter and urine bag) specifically for patients that want to stay active and transport the set conveniently in their daily life. A no-touch- system enables safe insertion of the catheter without the user having to touch the catheter itself. The intermittent technique shows great advantages in terms of reduction of urinary tract infections compared to a permanent catheter. It improves the life of patients suffering from body shame. Those patients, who can practice self-catheterization with the help of solutions such as Actreen®, will no longer have to cope with embarrassment and thus can enjoy an active social life.
Here you will find all sources used for the Annual Report 2017.
Protein, fat and glucose
Nutritional therapy | 33 million people in Europe suffer from malnutrition. And not because they have too little to eat, but rather because their body cannot absorb sufficient nutrients. Or because they need an unusual amount of energy due to illness. The elderly and people with cancer are particularly affected, as well as patients in intensive care units. Their bodies, already under attack, are further weakened. The energy requirements of an oncology patient are approximately tripled – and malnutrition is one of the most frequent causes of death.1 Nutritional therapy can help.
Goal of therapy
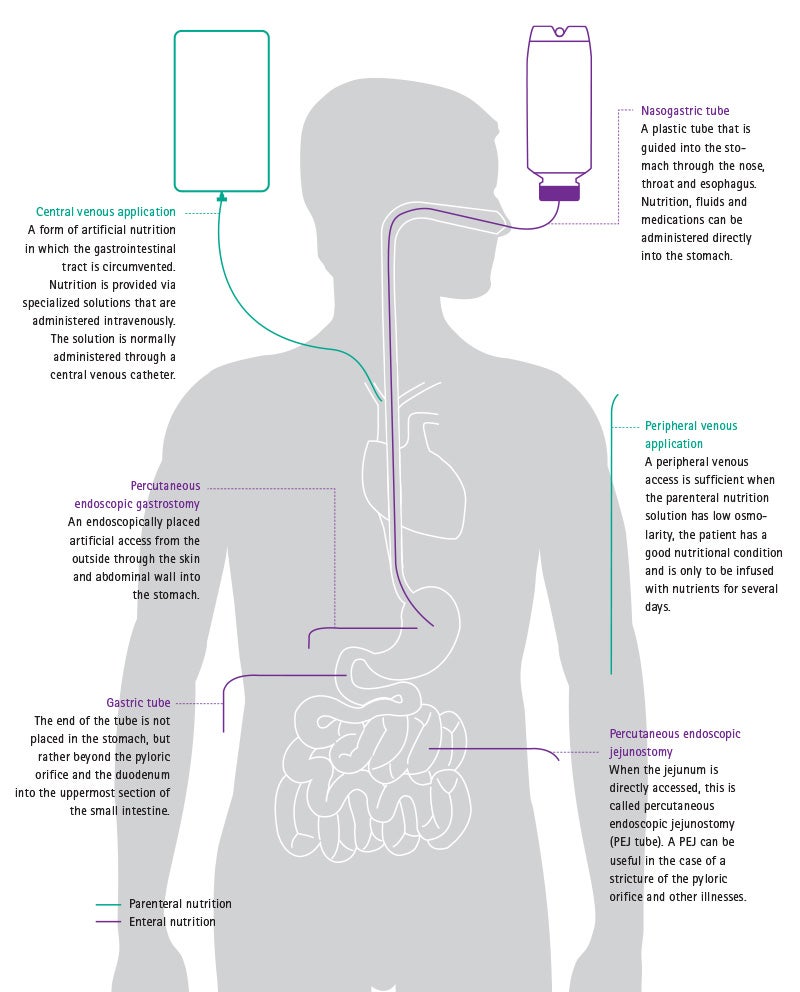
The goal of the therapy is always to establish or improve the nutritional state of the patient, so that the body has enough power and energy to live and to fight its disease. The necessary nutrients can be supplied in different ways (see illustration). For example, it is possible for patients to drink high caloric liquid nutrition in addition to normal nutrition – oral nutritional therapy. However, some patients cannot swallow or chew, suffer from severe nausea or are unable to keep food down. These cases can be helped by enteral therapy, in which the nutrition enters the stomach or small intestine directly via a tube. At B. Braun, with Nutricomp liquid and tube feed nutrition, we produce a full assortment for oral and enteral nutritional therapy. The corresponding treatments are not only performed in hospitals, but also in nursing homes or private residences. It is therefore important that the food bottles are sturdy and easy to handle. That's why they are produced from a particularly durable material.
Oral, enteral, parenteral
Oral or enteral nutritional therapy should always be the first method of choice. After some operations, however, the stomach can no longer transport food. With parenteral nutritional therapy, the basic components of food – glucose, protein and fat, as well as electrolytes, vitamins and trace elements – are injected directly into the bloodstream, circumventing the gastrointestinal tract. Parenteral nutrition therapy was inconceivable before the 1960s, and since then has saved countless human lives. The primary components of artificial nutrition must be stored separately from each other, to extend shelf life, and may only be mixed shortly before being administered. For a long time, the latter was the demanding task of a hospital pharmacist. Incidentally, the fight against malnutrition does not only help patients with acute ailments. Some illnesses, such as short bowel syndrome as a result of Crohn's disease, cause patients to be able to absorb only a portion of their nutrition via the intestine. The solution: parenteral nutrition, which can also be administered at night, or even while traveling, with a corresponding backpack. This allows patients to live an autonomous and active life despite what is actually a severe illness.