Are surgical instrument issues impacting your surgeries?
Disruptive factors in the operating room
The operating room (OR) is a key resource in all major hospitals, and the surgeon is at the heart of every operating room.
Surgery without a surgeon is impossible – the surgeon guides the operation while bearing responsibility for the well-being of the patient. But surgeons cannot operate with their bare hands. They not only depend on surgical instruments, but also on the right instruments that are in excellent condition. For this, every surgeon depends on the Central Sterile Supply Department (CSSD) and Operation Room Staff.
However, as CSSD processes are often far from optimal, surgical sets can be a strong disruptive factor in the OR. Missing or malfunctioning instruments are one of the leading causes of suboptimal surgical processes that result in delays, stress, mistakes and surgical site infections (SSIs). [1], [2]
A good reputation is vulnerable
Each incident in the OR damages the reputation of the responsible surgeon and costs valuable time, which is a rare asset of every surgeon. To be seen as a successful surgeon, specific KPIs have to be fulfilled, and patient well-being and satisfaction are indispensable for a good reputation. Having a good standing in the hospital is also vital for a surgeon: Colleagues should honor the surgeon’s work, and OR staff should enjoy working with the surgeon. All this is not always easy to achieve, especially when processes in the OR regularly fail to run smoothly.
What are the main threats?
Delays in the operating room
A benchmark study in 13 Dutch hospitals found that delays in the OR add up to around 2,150 lost hours or 270 lost days.
Anesthesia procedures as well as a poor scheduling and planning processes were identified as the most critical factors in this study. [3] However, a prospective study from Canada found equipment failure, including missing or malfunctioning surgical instruments, to be the most common cause for delays in the OR. [2] The reasons why surgical sets can negatively impact the surgical process and how this happens are not only well-known, but also, unfortunately, very diverse.
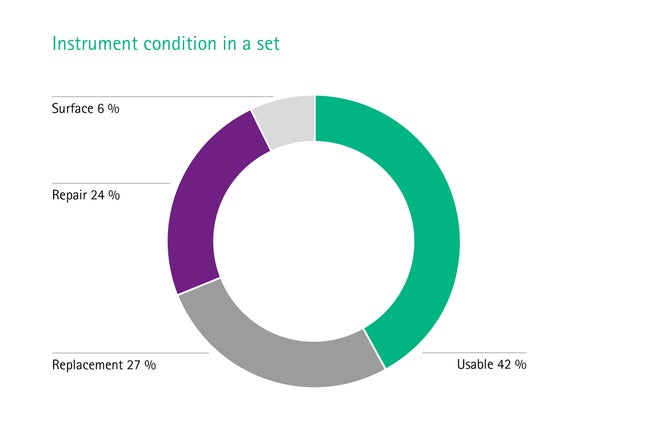
More than half of the instruments are in bad condition and unusable
On average, only 42% of the instruments within a set are fit for use, something you have surely experienced several times.
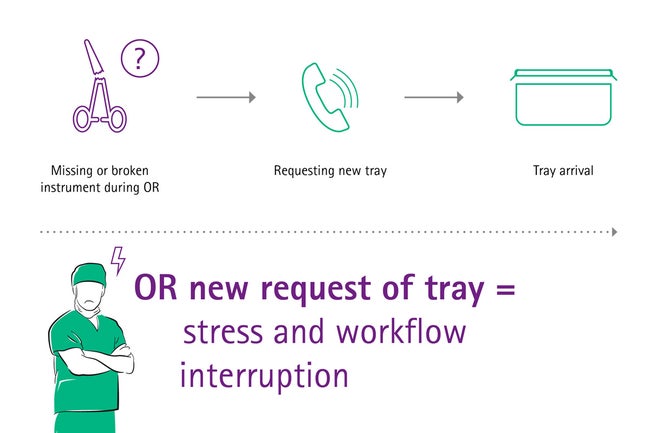
Often, more than half of a set needs either replacement (27%), repair (24%), or surface treatment (6%) due to corrosive effects. [4], [5] When a new tray has to be ordered during surgery, it takes roughly seven precious minutes to arrive in the OR. [2], [6] During this time, there is not much to do except wait. Prolonged duration of surgical procedures is associated with complications risk for patient. [7]
Surgical sets are often incomplete or incorrectly packed
As a surgeon, this is something you have probably experienced quite often: Although many sets are overloaded, they often contain the wrong instruments – but not what is needed. For example, it was reported that gynecological instruments were sometimes packed into trays for orthopedic operations by mistake. [8]
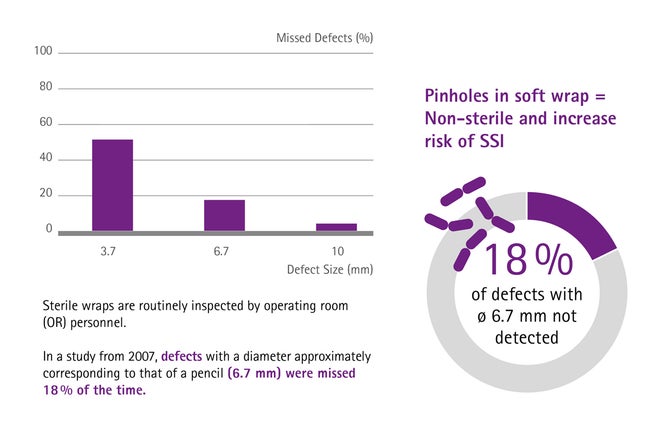
Soft wrap packing is a health hazard
The instruments are often packed in soft wraps, which are prone to pinholes if not handled appropriately, for example during stocking. When this happens and pinholes are detected in OR, the entire set is considered non-sterile and a new surgical set is requested, negatively affecting the workload in OR.
Even worse, regarding patient safety, 18% of pinholes are not detected by the medical personnel, [9] thus increasing the risk of SSIs. Although this is not your fault as a surgeon, you will be made responsible for complications.
The human factor
All these incidents are incredibly stressful for those involved – and stress is a hazard as it increases the rate of mistakes and may dampen the mood of the whole team. In addition, high stress levels cause illness, and it is especially health care workers who very often suffer the effects of work-related stress. [10]
While humans are known to make errors from time to time, the OR is not the place for it. Time and again, human error or poor communication leads to avoidable surgical incidents. Just as proper instrument management will help to ensure the appropriate technical conditions when operating, a well trained and focused OR-staff is an equally crucial part of a successful operation.
Performing successful surgeries with high-quality surgical instruments
What can be done to make your surgeries run smoothly?
A well-structured workflow in the CSSD and the OR as well as high-quality surgical equipment are essential for performing successful surgeries, guaranteeing patient safety, and increasing the number of treatable patients. Establishing smooth working routines prevents conflicts and errors, and makes processes more efficient. This will allow you to concentrate all your energy on your work as a surgeon and achieve excellent results.
How can you be supported in your work as a surgeon?
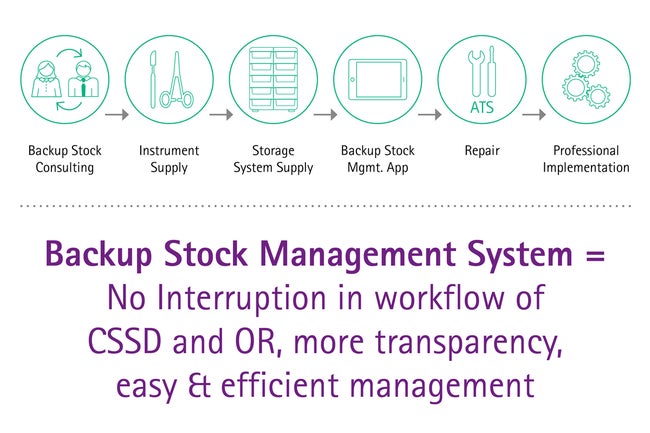
Maintenance, repair & back-up stock management
Ensuring the optimal functionality and availability of surgical equipment allows operations to go ahead as planned, avoiding delays, stress and costs. A professional high-quality repair management and a technical service that is reliable and always available when needed can help you to achieve the required functionality of the instruments. In addition, a good backup management guarantees that functioning devices are always available. This allows operations to go ahead as planned while other instruments require repair or maintenance.
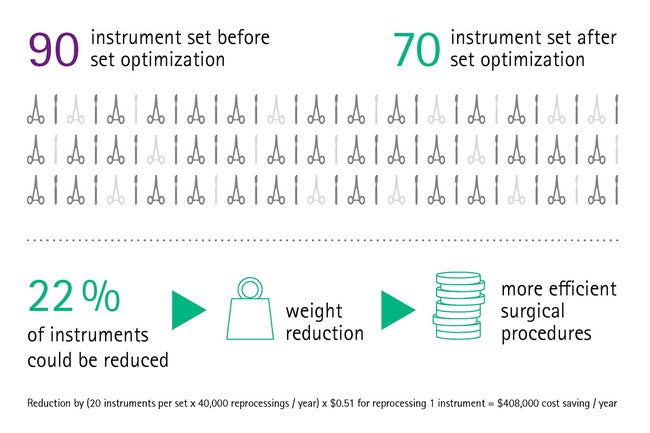
Set optimization
Our findings show that set optimization is a highly important and effective measure: Surgical sets are often overloaded or loaded incorrectly. But sets can be optimized and adapted for a variety of surgical procedures, [11] ensuring that you are provided with a set containing everything you need for an intervention, but nothing that is unnecessary. This prevents long searches for the required instrument or having to order missing instruments – and the operation can be performed smoothly.
Set packaging
We aim to minimize any risks that are inherent to soft packaging, such as the puncture hazard for OR staff or the loss of instrument sterility due to punctured bags. With the sterile container system we offer a safe and reliably sterile solution. Instrument sterility can easily be maintained and safe transport and storage of instruments is no longer an issue, ultimately reducing both the risk of surgical site infections and the stress associated with handling the vulnerable soft wrap packing.
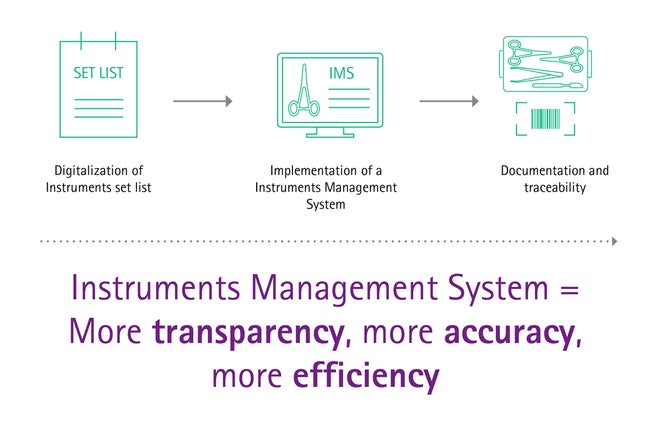
Digitalization and instrument management system
The global trend of digitalization is a driver of automation and efficiency. Recent advances made in these areas can also be of benefit for surgical asset management: Modern digital tray organizing solutions reduce assembling errors and workload in an easy and smart way. Also, IT support can control the majority of high-risk hazards in the entire delivery process of surgical instruments, [12] taking the strain off surgeons.
Staff training
Well-trained staff is a vital part of every department. Human error or poor communication are responsible for around twothirds of surgical incidents, with a total rate of fatal adverse events estimated at one per 10,000. [13] Professionally qualified staff will make fewer mistakes and can immediately identify possible hazards (e.g. contaminated instruments). When the staff is well-trained and you can rely on everyone’s work, you will be able to focus entirely on your own work.
At AESCULAP®, we know that surgeons are under tremendous pressure due to demanding operating room schedules. We also know how difficult it can be for a surgeon to gain and keep a good reputation – especially when you depend on factors you cannot influence. This is why we would be happy to support you with this issue, enabling you to achieve outstanding surgical results.
[1] Anderson, D.J., et al., Strategies to prevent surgical site infections in acute care hospitals. Infection Control & Hospital Epidemiology, 2008. 29(S1): p. S51-S61.
[2] Wong, J., et al., Delays in the operating room: signs of an imperfect system. Canadian Journal of Surgery, 2010. 53(3): p. 189.
[3] Does, R.J., et al., Reducing start time delays in operating rooms. Journal of Quality Technology, 2009. 41(1): p. 95-109.
[4] Aesculap statistics based on 345.890 analyzed instruments in 135 different hospital.
[5] Lunardini, D., et al., Lean principles to optimize instrument utilization for spine surgery in an academic medical center: an opportunity to standardize, cut costs, and build a culture of improvement. Spine, 2014. 39(20): p. 1714-1717.
[6] Stockert, E.W. and A. Langerman, Assessing the magnitude and costs of intraoperative inefficiencies attributable to surgical instrument trays. Journal of the American College of Surgeons, 2014. 219(4): p. 646-655.
[7] Cheng, H., et al., Prolonged operative duration is associated with complications: a systematic review and meta-analysis. Journal of Surgical Research, 2018. 229: p. 134-144.
[8] Jeffreys, B. NHS ‘chaos’ over surgical tools. 2008.
[9] Waked, W.R., et al., Sterilization wrap inspections do not adequately evaluate instrument sterility. Clinical Orthopaedics and Related Research®, 2007.462: p. 207-211.
[10] Ford, S. Exclusive: Stress levels at work making nurses ill, finds survey. 2014.
[11] Yoon, S., et al., Implementation and Impact of a Hospital-Wide Instrument Set Review: Early Experiences at a Multisite Tertiary Care Academic Institution. American Journal of Medical Quality, 2019. 34(1): p. 67-73.
[12] Guédon, A.C., et al., Where are my instruments? Hazards in delivery of surgical instruments. Surgical endoscopy, 2016. 30(7): p. 2728-2735.
[13] Catchpole, K., et al., Surgical Safety can be improved through better understanding of incidents reported to a national database. Nat Patient Safety Agency, 2009.